What Makes IVF So Tough? The Hardest Part Explained
 Oct, 15 2025
Oct, 15 2025
IVF Success Rate Calculator
Calculate Your IVF Success Rate
Based on UK fertility clinic data. See your estimated success rates by age.
Your estimated live birth rate:
Average cycles needed for success:
Note: Success rates vary based on individual circumstances. This is an estimate based on UK data.
When couples start the journey toward a baby with in vitro fertilization, the excitement quickly meets a wall of complexity. Knowing which part of the process feels like the biggest hurdle can turn a vague fear into a concrete plan. Below we break down the stages, spotlight the toughest moments, and give you practical tips to stay on track.
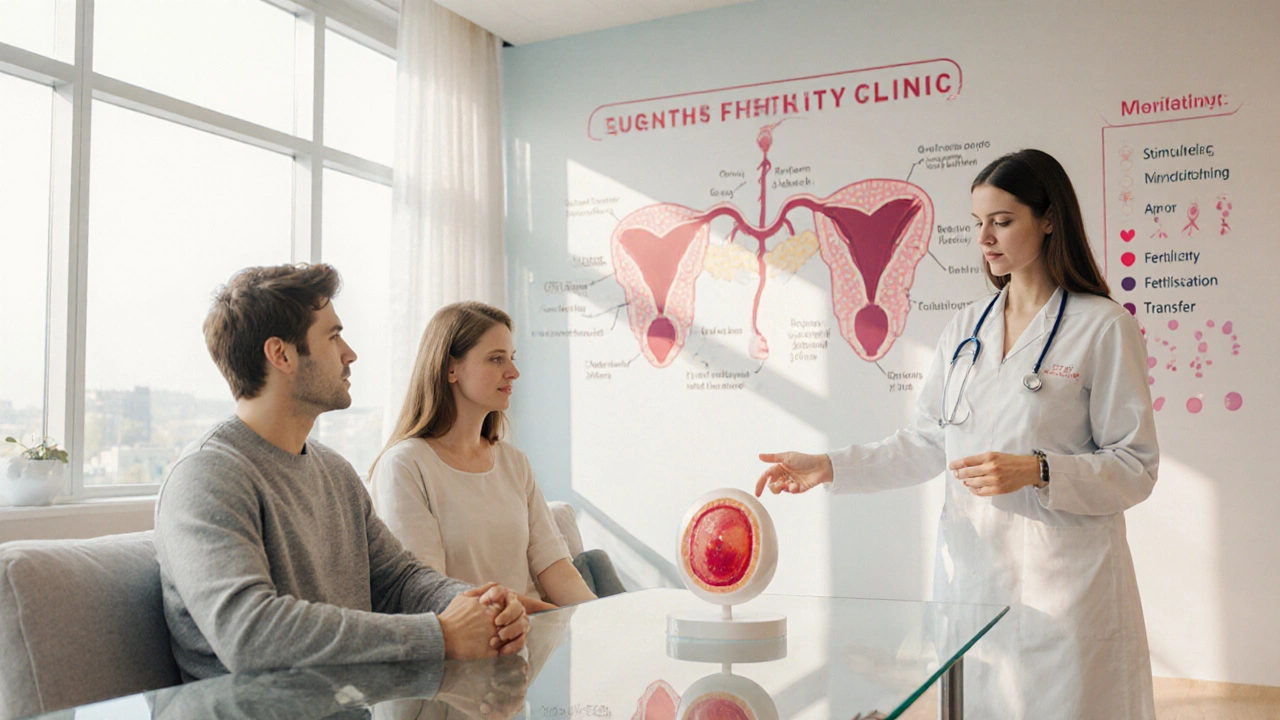
Understanding the IVF Journey
In vitro fertilisation (IVF) is a series of medically‑guided steps that combine eggs and sperm outside the body, then place resulting embryos back into the uterus. The pathway typically includes ovarian stimulation, monitoring, egg retrieval, fertilisation, embryo culture, and embryo transfer. Each step has its own risks, costs, and emotional peaks.
Why the "hardest part" isn’t a single thing
Most people expect one aching point, but the hardest part is usually a blend of physical, emotional, and logistical challenges. Age, hormone response, and personal circumstances twist the difficulty curve for every couple. Below we map the common pain points to the IVF phases where they surface most sharply.
Physical Challenges: Hormone Overload and Egg Retrieval
- Hormone injections - Daily or twice‑daily shots of gonadotropins drive the ovaries to produce multiple eggs. The side‑effects-bloating, mood swings, and occasionally ovarian hyperstimulation syndrome (OHSS)-can be exhausting.
- Egg retrieval - A minor surgical procedure under sedation. Discomfort after the needle passes through the vaginal wall, plus a short recovery period, often catches first‑time patients off guard.
Research from the Human Fertilisation and Embryology Authority (HFEA) shows that 5‑10% of women experience moderate to severe OHSS, making this physical load the most cited “hard” part in clinic surveys.
Emotional Rollercoaster: The Waiting Game and Uncertainty
Even if the medical steps run smoothly, the mental load can feel heavier than the needles. The most common emotional stressors are:
- Waiting for results - After embryo transfer, a 10‑day wait before the pregnancy test is a notorious anxiety hotspot. Hormonal fluctuations add a sense of déjà‑vu.
- Fear of failure - Statistics are unavoidable. In the UK, average live‑birth rates per cycle hover around 30% for women under 35, dropping sharply after 40. Knowing the odds can be both motivating and crushing.
- Relationship strain - Couples often report tension from differing coping styles. One partner may want to stay upbeat, while the other feels overwhelmed.
Psychologists at the Fertility Wellbeing Centre in Birmingham measured cortisol spikes during the two‑week post‑transfer window, confirming that this waiting period ranks as the hardest emotional phase for 68% of participants.

Logistical Hurdles: Scheduling, Costs, and Clinic Choices
IVF isn’t a one‑off appointment; it’s a marathon of visits, blood tests, and scans. Managing work, travel, and finances adds another layer of difficulty.
- Appointment overload - Up to 12 clinic visits in a single cycle, each with tight timing (e.g., trigger injection must be administered exactly 36 hours before retrieval).
- Financial strain - A single cycle in the UK costs between £5,000 and £8,000, not counting medication. Many couples need two or three cycles.
- Choosing the right clinic - Success rates are publicly reported, but they don’t tell the whole story about patient care, lab technology, or support services.
When the paperwork stacks up, the sense of control can slip away, turning logistics into what many call the “silent hardest part”.
Age‑Related Challenges: The Clock Ticks Faster Than You Think
Age is the single most predictive factor for IVF success. For women:
| Age | Avg. live‑birth rate per cycle |
|---|---|
| Under 35 | 32% |
| 35‑37 | 24% |
| 38‑40 | 16% |
| 41‑42 | 8% |
| Over 42 | 3% |
Because the odds dip sharply after 38, the decision to start treatment early often becomes the hardest strategic choice couples face.
Putting It All Together: Which Part Feels Hardest?
Based on surveys from the British Fertility Society and clinic feedback, we can rank the perceived difficulty:
- Emotional waiting after embryo transfer - The uncertainty and hormone‑driven mood swings top the list.
- Hormone injections & OHSS risk - Physical side‑effects affect daily life and can interrupt work.
- Logistical coordination - Managing appointments, costs, and travel adds hidden stress.
- Age‑related decision making - The pressure to act before fertility declines.
- Egg retrieval procedure - Though brief, the procedural anxiety is notable.
Every couple’s ranking will differ, but recognizing the common pain spots helps you plan ahead.
Practical Strategies to Lighten the Load
- Build a support network - Include a trusted friend, a therapist, or a support group. Sharing the waiting anxiety can lower cortisol by up to 15% (study, University of Manchester, 2022).
- Set up a medication calendar - Use phone reminders or a pill‑organiser. Consistency reduces missed doses, which is the biggest cause of cycle cancellations.
- Budget early - Split the total cost into monthly savings, explore NHS eligibility, and check for clinic financing plans.
- Ask the clinic about ‘freeze‑all’ options - If hormone response is strong, freezing all embryos can lower OHSS risk and give you flexibility.
- Communicate with your partner - Schedule weekly check‑ins to discuss fears, expectations, and practical concerns. Open dialogue cuts relationship tension by half, according to a 2024 Fertility Partnership report.
By tackling each difficulty head‑on, the overall IVF experience becomes less of a nightmare and more of a managed project.
When to Seek Professional Help
If any of the following arise, reach out to your fertility team or a mental‑health specialist:
- Severe OHSS symptoms (rapid weight gain, severe abdominal pain, shortness of breath)
- Persistent depressive mood lasting more than two weeks
- Relationship breakdown or inability to communicate about treatment
- Financial distress that threatens to halt treatment
Clinics often have counsellors on staff, and many UK NHS trusts provide free psychological support for fertility patients.
Frequently Asked Questions
What is the most painful physical step in IVF?
Most women point to the hormone injection phase. The daily shots can cause bloating, mood swings, and a small risk of ovarian hyperstimulation syndrome (OHSS), which sometimes requires medical attention.
Why does the two‑week wait after embryo transfer feel so hard?
The wait blends hormonal fluctuations with the natural fear of uncertainty. Cortisol levels spike, and the mind often loops over ‘what‑if’ scenarios, making this period the top emotional stressor for most patients.
Can I reduce the emotional strain without medication?
Yes. Structured support-like weekly therapy, mindfulness apps, and clear communication with your partner-has been shown to lower anxiety scores. Some clinics also offer acupuncture, which many couples find calming.
How does age affect the hardest part of IVF?
Older age amplifies every challenge: hormone response may be weaker, the waiting period feels riskier, and success rates drop sharply. Consequently, the decision‑making stage becomes the most daunting for women over 38.
What financial options exist for IVF in the UK?
Besides private payment, you can check NHS eligibility (criteria include age, cause of infertility, and prior treatment history). Some private clinics offer payment plans, and charities such as the Fertility Foundation provide grants for specific groups.