How to Poop After Knee Replacement Surgery: A Practical Guide
 Dec, 16 2025
Dec, 16 2025
Post-Surgery Bowel Health Calculator
This tool estimates your constipation risk based on key factors from clinical guidelines. It's not medical advice - always consult your care team.
After knee replacement surgery, you’re focused on walking, swelling, and pain. But one thing no one talks about until it hits you? pooping. It’s awkward, uncomfortable, and surprisingly common to struggle with bowel movements after surgery. If you’re wondering how to poop after knee replacement surgery without hurting your knee or risking complications, you’re not alone. Millions of patients face this every year-and it’s totally fixable with the right approach.
Why is it hard to poop after knee replacement surgery?
Your body isn’t broken-it’s just slowed down. Surgery triggers a stress response. Your digestive system pauses to redirect energy toward healing. Add to that:
- Pain meds like opioids (oxycodone, hydrocodone), which are notorious for slowing gut movement
- Reduced movement-you’re not walking like before, so your intestines aren’t getting the natural squeeze they need
- Dehydration-many patients drink less water because they’re afraid of needing to pee often or because they’re not hungry
- Diet changes-hospitals serve bland food, and you might be eating less fiber-rich meals
These factors combine to make constipation the #1 complaint after knee replacement, even more than pain in some cases. Studies show up to 70% of patients experience significant constipation in the first week after surgery. That’s not normal-it’s preventable.
What happens if you don’t fix it?
Ignoring constipation isn’t just uncomfortable. Straining too hard can:
- Put pressure on your new knee joint, causing pain or swelling
- Trigger muscle spasms in your thigh or hip, making physical therapy harder
- Lead to hemorrhoids or anal fissures, which are painful and slow healing
- In rare cases, cause bowel obstruction or fecal impaction, requiring medical intervention
You don’t want to risk delaying your recovery because you didn’t address a simple issue. The goal isn’t to poop every day-it’s to poop easily, without strain, every 1-3 days.
Step-by-step: How to poop after knee replacement surgery
Here’s what actually works, based on real patient experiences and clinical guidelines from NHS physiotherapists and orthopedic nurses.
- Start hydration before surgery-Drink at least 2 liters of water daily in the week leading up to your operation. Don’t wait until after to start.
- Keep drinking after surgery-Aim for 8-10 glasses a day. Add lemon or ginger to water if plain water makes you nauseous. Herbal teas like peppermint or chamomile count too.
- Move your body-Even if you’re in a wheelchair or on crutches, wiggle your toes, roll your ankles, and do seated marches. Movement stimulates your bowels. Get up and walk short distances as soon as your nurse says it’s safe.
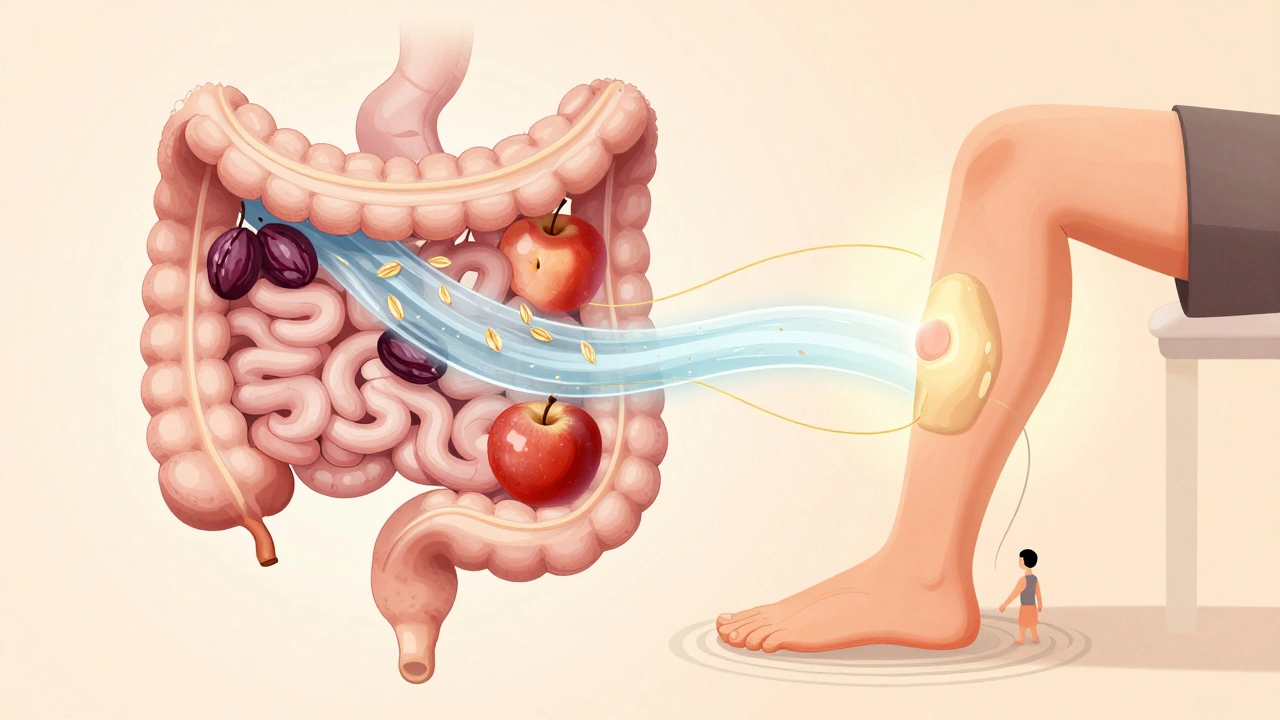
- Eat fiber-rich foods-Prunes, apples (with skin), oats, beans, and bran cereal are your friends. If solid food is hard to eat, try prune juice (half a cup daily) or blended fruits like pear or mango.
- Use stool softeners, not laxatives-Doctors usually prescribe docusate sodium (Colace) after surgery. It softens stool so you don’t have to strain. Take it daily for the first 7-10 days. Avoid stimulant laxatives like senna unless your doctor says so-they can cause cramping and dehydration.
- Position yourself right-Sitting on the toilet with your knees higher than your hips helps. Use a small footstool under your feet. Lean slightly forward. Don’t hold your breath or push hard. Let gravity do the work.
- Use your hands wisely-If you’re worried about bending your knee, place a pillow between your legs to keep them slightly apart. You don’t need to squat. Just sit comfortably and relax.
- Time it right-Try to go about 20-30 minutes after meals. That’s when your colon naturally activates. Don’t wait until you’re desperate.
What to avoid
Some common advice actually makes things worse:
- Don’t rely on enemas-They’re invasive, can irritate your rectum, and aren’t needed unless you’re completely stuck for over 5 days.
- Don’t take extra painkillers-More opioids = more constipation. Ask your doctor about switching to non-opioid pain relief (like acetaminophen) as soon as possible.
- Don’t wait-If you haven’t pooped in 4 days, call your surgeon’s office. Don’t suffer in silence.
- Don’t force it-Straining can damage your surgical site, even if your knee feels fine. If you feel pressure or pain, stop. Try again later.
When to call your doctor
Constipation is normal. A blockage isn’t. Call your surgeon if you have:
- No bowel movement for 5 or more days
- Severe abdominal bloating or cramping
- Vomiting or inability to pass gas
- Blood in your stool (not just from hemorrhoids)
- Fever or chills along with constipation
These could signal a bowel obstruction or infection. It’s rare, but it happens-and it needs quick attention.

Real patient tip: What actually helped
One patient in Birmingham, 72, had knee replacement in October 2025. She started taking prunes daily before surgery and kept a small stool next to her toilet. She drank a glass of warm water with lemon every morning before getting up. She didn’t use laxatives. By day 3, she was pooping without pain. Her physiotherapist said her recovery went faster because she wasn’t distracted by constipation.
Another man, 68, was terrified to move after surgery. His nurse gave him a simple rule: “If you can move your toes, you can move your bowels.” He did seated leg lifts every hour. By day 2, he was regular.
The message? Small habits make a big difference.
What about bowel control or incontinence?
Some people worry they’ll lose control after surgery. This is rare. Nerve damage from knee replacement is extremely uncommon. If you notice sudden incontinence, tell your doctor immediately-it’s not normal and needs checking. Most people just feel less control because they’re afraid to strain or because they’re on pain meds that affect muscle tone. This usually clears up in a few days.
Long-term: Getting back to normal
Once you’re off opioids and back to walking regularly, your bowels will return to normal. Most patients report full bowel regularity by 4-6 weeks. Keep eating fiber, stay hydrated, and keep moving. You might even find you’re more regular than before surgery because you’re paying attention to your body.
Don’t let embarrassment stop you from talking to your care team. Nurses and doctors have seen this a thousand times. They’re not judging you-they’re there to help you heal faster.